Breast Cancer Screening: Thermogram No Substitute for Mammogram
August 1st, 2020
Cyrus Khorrami, MD
Radiologist, Medical Director
About 1 in 8 women will be diagnosed with breast cancer sometime in their lives, reports the National Cancer Institute, part of the National Institutes of Health. Rarely, men also can have breast cancer. But there has been a decline in breast cancer deaths in recent years, and one reason is because cancers have been detected earlier through mammography, according to the American Cancer Society. Breast cancer is among the leading causes of death among women between 25 and 65 years, with an expected incidence of 1 in 8 women in most countries. Screening and early diagnosis are still the best way to reduce the number of breast cancer deaths. However, there can be some misinformation over the best method of screening patients for this disease.
On behalf of the Radiologists at Toms River X-Ray, I wanted to remind you that mammography is still the most effective breast cancer screening test. Proper breast cancer screening lets health care providers check for cancer even before there may be signs and symptoms of the disease.
About mammography
Mammography is a radiographic method which uses low-dose X-rays to image the breast tissue for both screening and diagnosis of breast cancer. Any suspicious high-density regions or unusual patterns such as microcalcifications are examined carefully. Suspicious findings could be due to a range of abnormalities, such as tumors (benign and malignant), areas of scarring, or cysts with solid areas.
Mammograms do not prevent breast cancer, but they can save lives by finding breast cancer as early as possible. Mammography is a fast procedure (about 20 minutes), and discomfort is minimal for most women. The procedure is safe: there is only a very tiny amount of radiation exposure from a mammogram.
Does the radiation in mammograms cause breast cancer?
Mammograms expose you to low-dose radiation, causing little to no risks. There are no reliable studies that show the radiation in mammography causes breast cancer. The radiation dose is very low and for most women the benefits of regular mammograms outweigh the risks posed by this tiny amount of radiation.
Why do you need to compress the breast in mammograms? Can that spread potential breast cancer?
Breast compression is important to spread the breast tissue around to expose potential underlying cancers. There is a 100 year old myth that compressing the breast can spread potential breast cancer. That is utterly false that there is no reliable evidence or data shows this.
In addition, mammograms aren't 100% accurate and factors — such as your age and breast density — may result in false-negative or false-positive mammograms.
About thermography
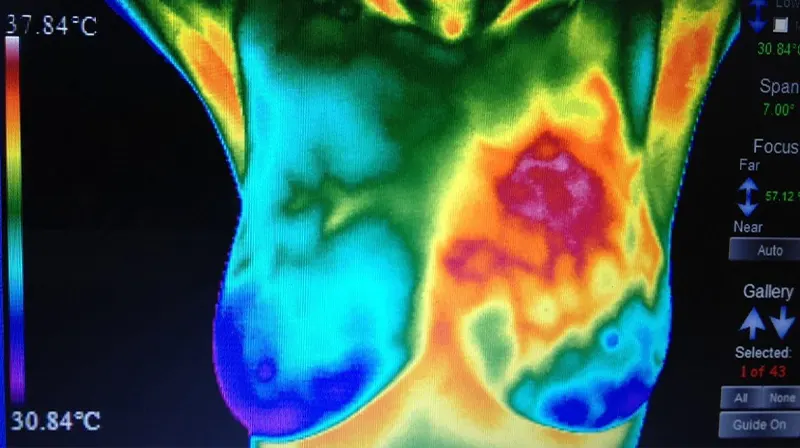
Thermography is an imaging procedure that screens for cancerous tissue using temperature differences at the breast surface, detected by infrared cameras. The theory is malignancies are usually warmer than normal tissue, leading to increased blood flow through the tumor, as well as the higher rate of metabolism in cancer cells.
Thermography pros and cons
Thermography is appealing because it is non-invasive and does not involve radiation exposure. In addition, it is capable of picking up asymmetric increases in heat in the breasts, which could alert women to the need for serial screening years before a cancer is detectable by mammography.
Why is thermography not the preferred method of breast cancer screening?
The heat recordings of thermography may change with inflammation, infection, exercise, or sometimes hormonal changes. Thermography is not adequate for certain situations like older or morbidly obese women, those with larger cancers, breast implants and large or pendulous breasts. The sensitivity and specificity of thermography are still not comparable to those of mammography as it cannot pick up very small cancers or those buried in the breast tissue.
At present, the detection rate for thermography is only 42% to 80% of cancers, as against 82% to 93% with mammography. Its false positive rate is 25%, more than double that of mammography.
Because of these lower detection rates, the FDA cites thermography as an adjunctive or additional tool which should not be used alone to rule out breast cancer. Patients who wish to undergo a thermography test should do so in conjunction with mammography.
Advice for patients getting a breast cancer screening
If you are worried about having a mammogram, talk to your health care provider about what you can expect. Also talk to your health care provider if you have specific questions about mammography, including questions about when and how frequently you should be screened. As a rule, you should also call your health care provider if you notice any change in either of your breasts such as a lump, thickening or nipple leakage, or changes in how the nipple looks. To schedule a breast cancer screening call Toms River X-Ray today: (732) 244-0777